Dallas scientists granted $420K to test gene therapy for rare neurological disease

Childhood-onset striatonigral degeneration is a rare genetic disorder that robs children of the ability to walk and speak by age five. Affecting anywhere between one to nine out of a million people, the often fatal disease has no cure. But geneticist Jonathan Rios is determined to change that.
For two years, the director of molecular genetics at Scottish Rite for Children has worked with colleagues at UT Southwestern to develop a gene therapy that reverses childhood-onset striatonigral degeneration in mice. Now, with a $420,000 grant from the National Institutes of Health, Rios is preparing to test whether it could do the same for children.
“I’d say 90% of the work we do [in the lab] is in rare conditions, patients that have conditions no one else is studying,” Rios said. “For example, our biorepository has collections of tissue samples from patients with a one-in-a-million condition. That [collection effort] is just part of what Scottish Rite is known for — the care — and that feeds a lot of what we do in terms of research.”

Discovered in 2016, childhood-onset striatonigral degeneration is a neurodegenerative disease involving a gene called VAC14 found on chromosome 16. This gene, Rios said, codes for a protein regulating osmotic pressure — or the pressure determining fluid movement across a cell membrane — inside cells of the central nervous system, which includes the brain and spinal cord. When VAC14 mutates and is passed down to a couple’s child, neurons in the brain develop holes, looking a bit like they’re filled with soap bubbles.
“When the pressure is not maintained, [neurons] develop these bubbles,” Rios said. “The bubbles get so large that it leads to cell death in the brain, in the spinal cord and elsewhere.”
A child has to inherit two copies of a mutated VAC14 gene from each parent for the neurodegenerative disease to cause damage — what’s called an autosomal recessive disorder. As its name suggests, symptoms associated with childhood-onset striatonigral degeneration appear during infancy or early childhood. These symptoms include dystonia, where a person will have involuntary muscle contractions that may force the body into repetitive, twisting and often awkward postures.
Affected children will also have difficulty swallowing and speaking because of weakened muscles. Eventually, the child loses its ability to speak and move entirely. The disease typically results in a short life expectancy.
“The disease can progress pretty rapidly,” Rios said. “There are families that are reported where you have a happy, healthy 2-year-old that, by age 3, is completely dependent on external care [and support]. So it’s very rapid onset in humans.”
Rios and his colleagues at Scottish Rite and UT Southwestern became interested in studying childhood-onset striatonigral degeneration in their quest to come up with gene therapies for inherited forms of spastic paraplegia that are associated with lower limb weakness and tightness.

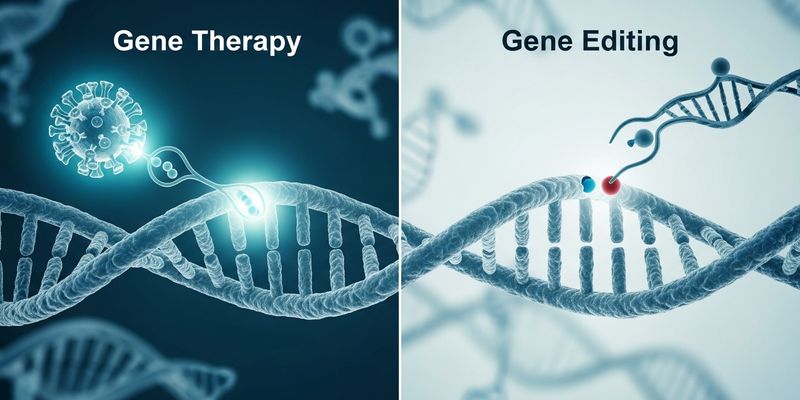
With the help of Dr. Bruce Beutler, director of UT Southwestern’s Center for the Genetics of Host Defense, the researchers created a mouse model of the neurodegenerative disease. They then engineered a gene therapy that uses a virus, rendered harmless and not infectious, to deliver a normal version of VAC14 into neurons and nerves.
“We’re giving [VAC14] back in hopes that we can better regulate pressure and not lose all those nerve cells,” Rios said. “If we can do that, then theoretically, all the manifestations of the disease should be erased.”
Results so far have been promising. In week-old mice with minimal neurodegeneration, a single treatment injected into the spinal cord prevented the disease from progressing.
“We completely rescued their overall health in terms of body weight; they have completely normal strength,” Rios said. “They are just as active and can walk on the wheel for just as long as completely normal mice.”
The development of the gene therapy and studies in mice were funded by Scottish Rite. Now, with the NIH funding, Rios plans to do more testing, with a goal of submitting an application to the U.S. Food and Drug Administration for an investigational new drug, the term for a substance that has been tested in a lab and approved for testing in humans.
“What we have to do now is test a dose in mice that is equivalent to what a human would receive,” Rios said. “We want to test whether that dose is effective and then we also have to test low doses … to see how low a dose we can provide that is still therapeutically effective.”
Because of the rarity of childhood-onset striatonigral degeneration, finding enough patients for clinical trials may prove tricky. But Rios is hopeful he and his colleagues will be able to do so and that FDA approval of their gene therapy may lead to the disease being identified and treated sooner.
“Our goal would be that if we can say for [childhood-onset striatonigral degeneration] that we have an effective gene therapy that can potentially provide a lifelong cure, that maybe it would be included in newborn screening,” Rios said. “Our goal is to identify patients. Right now, we can only identify them after they’re already presenting with symptoms, in which case it might be too late.”
Steven Gray, co-director of the UT Southwestern Medical Center’s Gene Therapy Program, agreed that establishing a gene therapy could eventually allow for the disease to be included in newborn screening. (Gray’s lab provided the virus that delivers VAC14 back into cells.) Like Rios, Gray anticipates the gene therapy will meet a profound need for a disease with no cure, as is the case with many rare genetic diseases.
How curative the gene therapy will be will depend on variables such as the extent and severity of neuron or nerve damage, which can’t be fixed, Gray said. “A lot depends on how early we can intervene … What we aim for is very meaningful treatment.”
Miriam Fauzia is a science reporting fellow at The Dallas Morning News. Her fellowship is supported by the University of Texas at Dallas. The News makes all editorial decisions.
link